Aging brings a lot of changes to the human body, and this includes diseases developed overtime from poor health choices, bad diet, repetitive movement, stress, etc. One of the most common chronic disabilities associated with aging is Degenerative Spine Disease (DSD), which often occurs to adult working population and a common reason for MRI referrals. Pain can occur from muscles, nerves, bones, ligaments, intervertebral disks and even paravertebral tissues.
DSD doesn’t refer to specific condition of the spine, rather, it is a general term that includes different types of disorders that can happen simultaneously on a patient.
Symptoms of Degenerative Spine Disease
- Back pain is usually intensified by twisting, lifting, and bending
- Lower back pain usually worsens through sitting
- Walking and running feels better than prolonged standing or sitting
- Changing of position alleviates pain
Different Types
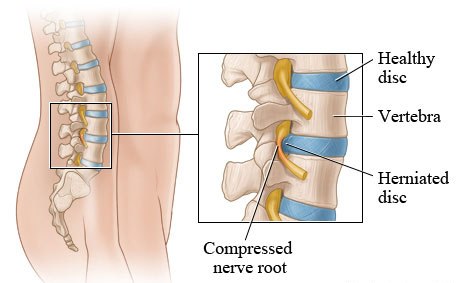
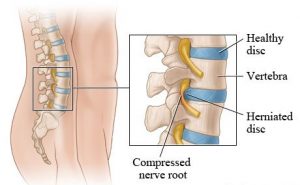
Herniated Discs
Herniated disc takes place between the spine’s vertebral bones. It is characterized by a protrusion, which can suddenly happen from trauma, but in most cases is developed over years. The most common areas for herniated disc is the lower back (lumbar herniated disc) and neck (cervical herniated disc), while can also happen in mid-back (thoracic herniated disc).
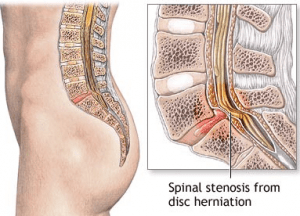
Spinal Stenosis
Spinal stenosis is characterized by narrowing of spinal canal, where the spinal cord sits, from the building up of tissue the covers the spine. It can also compress the nerves and the spinal cord. Spinal stenosis is usually lumbar (lower back) and cervical (neck) condition.
Degenerative Disc Disease
The spine is stabilized by the ligaments and muscular support, and moves in certain ways. In severe cases of DDD however, the stabilizers of the spin becomes lax, leading to weakness in certain areas. This instability leads to pain, which often leads to injury on the spinal cord and/or spinal nerves, which are both caused by neurological symptoms. Spinal instability is caused by trauma, tearing the supporting soft tissues or can even break the bones of the spine.
Examination Techniques for Degenerative Spine Disease
Most back pain and neck pain respond to conservative therapy, but for severe cases where unrelenting pain occurs, or associated with myelopathy or radiculopathy, MRI scan is needed to pin point and look for treatable cause.
Different anatomic sites are imaged in DSD, this includes the spinal cord, spinal canal, intervertebral disk, nerve roots, face joints, neuroforamina, and soft tissues that surrounds the spine. Generally, the spine is imaged in at least two planes, surface coils are almost exclusively used.
For cervical and thoracic regions, doctors will suggest T2-weighted sequence to search for and assess any damages on the spine.
To visualize neroforamina, thin sections are required, while pulse sequence is needed to counteract the CSF flow and physiologic motion.
For most cases, T1-weighted sequence and some type of T2 is required to get a myelographic effect. FSE (Fast spin-echo) technique can help save time compared to the conventional spin echo for T2-weighted imaging for the spine.
3D gradient-echo (GRE) method can get slice thicknesses 1mm or less, which can be an advantageous examination for showing cervical neuroforamina.
For postoperative spine cases, gadolinium injection accompanied with T1-weighted imaging is important to evaluate the improving lesions. Fat-suppression also helps in eliminating competing fat signals from other soft tissues and the bone marrow.
Treatment
Treatments for DSD vary from the specific area of the disease. Conservative therapy, rest and spine surgery are the common choices for treatment.

 I love to write medical education books. My books are written for everyone in an easy to read and understandable style.
I love to write medical education books. My books are written for everyone in an easy to read and understandable style.