CHAPTERS
Navigate to chapter
► Chapter 1: Disc Disease Overview
► Chapter 2: Disc Disease By Region
► Chapter 3: Standard Medical Treatments
► Chapter 4: Alternative Treatments and Self-Care
► Chapter 5: Nutrition and Spinal Health
Chapter 1: Disc Disease Overview
The phrase “disc disease” is misleading. This condition is a natural consequence of aging. The degeneration refers to alterations in the composition and function of the spinal cartilage, not necessarily to a progressive worsening of the accompanying symptoms.
When degenerative disc disease (DDD) is actively symptomatic, the problems it causes are typically located in the neck and/or lower back. The condition is highly variable in nature.
In some cases, the individual is completely unaware of its presence, and in others symptoms may actually improve depending on how the problem is addressed.
The Structure of the Human Spine
The spinal column is responsible for keeping humans upright, and is the center of our skeletal system. The length of the spine varies by height, but on average it will be 28 inches (71 cm) in men and 24 inches (61 cm) in women.
The Spinal Vertebrae
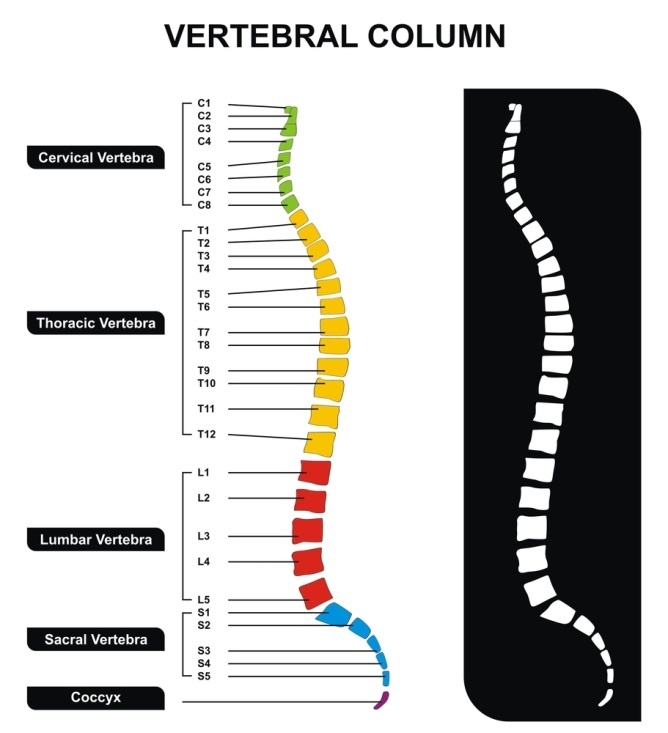
A total of 26 bony “blocks” or vertebrae separated by cushioning discs form the structure of the spine, which is divided into distinct regions:
– The cervical region or neck is composed of seven vertebrae. It is the most flexible portion of the spine.
– The thoracic region or mid-back includes 12 vertebrae.
– The lumbar region, or lower back, involves five vertebrae.
Below the last lumbar vertebrae, there are five more sacral vertebrae fused into the sacrum bone that run to the mid-buttock region of the body. Below that, lies the coccyx or tailbone. These are the least flexible portions of the overall structure.
If you were to view the spine from the side, it does not make a straight line, but rather follows four curves. The neck (cervical) and lower back (lumbar) portions curve inward, while the upper back (thoracic) and base (sacral) curve outward.
The curves stabilize and strengthen the total spine and help humans to remain balanced in our upright, standing position. The vertebrae grow larger toward the base of the spine because there they carry more weight.
The Function of the Discs
There are 23 discs that lie between the vertebrae that are designed to act as cushions, minimizing the impact of our daily movements on the spinal column. These structures also allow the spine to rotate and to move sideways.
There are no discs present between the skull and the first vertebra, or between the first and second vertebrae themselves.
Often you will see the discs compared to jelly donuts because they have a soft center called the nucleus pulposus. Each disc is a cartilaginous joint that compresses and decompresses (becomes thinner and thicker) as pressure is applied to it throughout the day.
At night, the discs get a chance to rest. Humans will always be slightly taller if measured in the morning than in the evening by a variation of about 1.5-2 cm.
An outer ring, the annulus fibrosus, which is comprised of ligaments, keeps the soft inner core contained so it can serve as a shock absorber.
The Spinal Cord
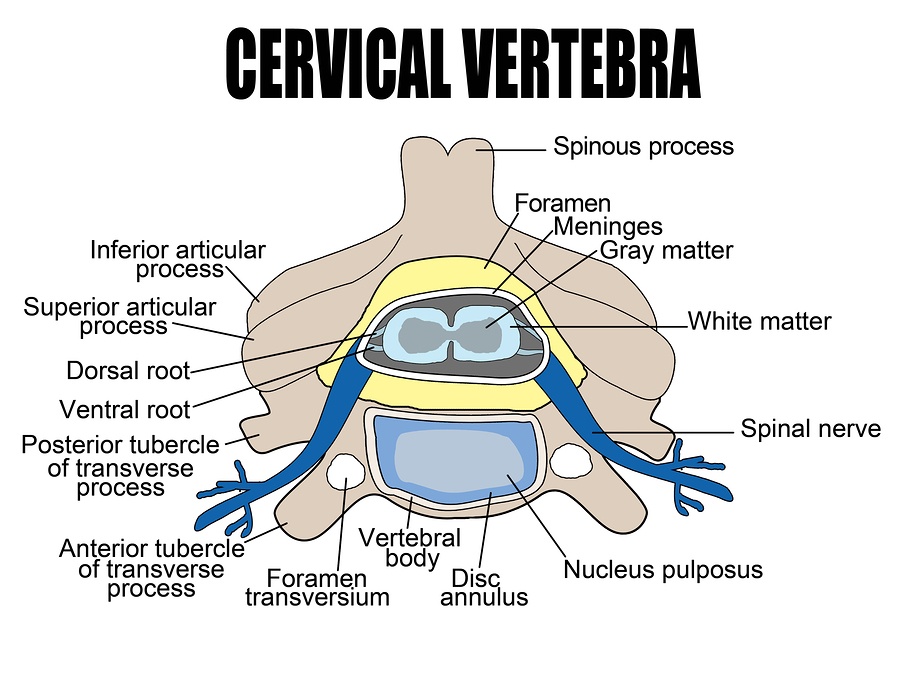
The spinal cord is encased in the center of the spine for protection. Each vertebra incorporates structures that allow spinal nerves to exit out of the spinal canal and branch outward.
These spinal nerves are responsible for carrying signals from the brain to the muscles and internal organs, and for relaying back sensory information gathered in the body.
This includes the ability to:
– feel heat and cold
– sense vibrations
– distinguish dull and sharp sensations
– sense the position of the limbs (arms and legs)
Additionally, the spinal cord plays a key role in the regulation of blood pressure, heart rate, and body temperature.
If these nerves are damaged, the effect can be extensive. Injuries to the cervical nerves (C1-C8) can result in quadriplegia, affecting the movement of the arms, hands, and legs. Damage to the thoracic nerves (T1-T12) may cause paraplegia, affecting the motion of the legs.
This complex interaction of the brain, spinal cord, and spinal nerves forms the body’s central nervous system. Often the symptoms of degenerative disc disease include neurological deficits like tingling in the extremities when some of these nerves become compressed.
When Degeneration Sets In
As humans age, the discs that separate the spinal vertebrae change in composition and size, leading to greater curvature of the spine. This explains why we become shorter as we get older.
Inflammatory Disc Pain
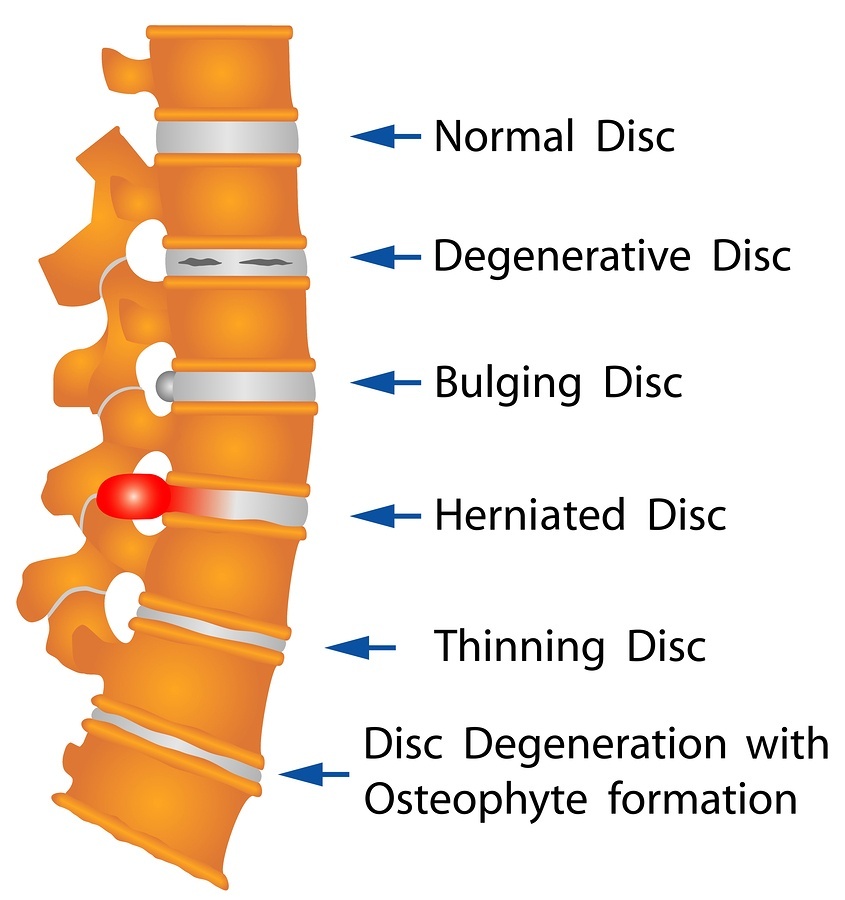
The principle alteration in the structure of the discs involves protein and water. As both are lost, the discs thin and weaken, losing their flexibility. These diminished capacities make the discs less effective as shock absorbers.
Discs have no way to repair themselves because they do not have their own blood supply. In fact, the discs don’t have many nerve endings, but the adjacent annulus fibrous does.
The proteins that leak out of the interior of the disc are inflammatory in nature, and are thus responsible for one type of pain that accompanies the degenerative process. The pain can also be mechanical, however.
 Mechanical Disc Pain
Mechanical Disc Pain
When disc pain is mechanical, a nerve root is being physically compressed, typically as a result of a herniation due to tears in the annulus.
The disc’s inner “jelly” gets forced outward, causing the disc to bulge (herniate) and sometimes to rupture. If enough fluid leaks out of the center of the disc, it may collapse.
The more the distance between the vertebrae shrinks, the less the bones are cushioned from the impact of movement and the less flexible they become.
Spinal Stenosis
The collapse and decompression of the spine can lead to spinal stenosis. This narrowing of the spine’s open spaces puts further pressure on the spinal cord and nerves, and happens most commonly in the neck and lower back.
Additionally, the facet joints located between and behind the vertebrae for stabilization may begin to shift. Normally, these joints are in almost constant motion, but with spinal decompression, the bone may begin to overgrow leading to the development of bone spurs.
Bone Spurs
Bone spurs or osteophytes are the body’s attempts to stop excessive and painful spinal motion, but if the spurs grow into the spinal canal, they begin to press on the nerves causing even more pain.
Thus, the degeneration that begins with water loss in the joints can move through a progressive alteration of healthy spinal function with a cascading set of painful symptoms.
Exacerbating factors in this progression include, but are not limited to:
– being overweight
– having poor posture
– lifting heavy objects on a regular basis
– being subject to repetitive motion
– smoking
Generally, the progression of degenerative disc disease is so slow people don’t realize the discs in their spines are changing. Rarely is the condition so severe as to require surgery.
On the other end of the spectrum, however, pain may be sufficiently debilitating to limit daily activities. This pain may present in the lower back or neck, but can also radiate into the shoulders, arms, buttocks, and legs. Twisting and reaching upward typically make the discomfort worse.
Diagnosing Degenerative Disc Disease
A diagnosis of degenerative disc disease starts with an extensive medical history. This will include questions about:
– symptoms (past and present)
– the pattern of change in those symptoms
– past injuries or illnesses
– treatment or intervention for past illnesses and injuries
– descriptions of current and past activities
During the course of the examination, the doctor will test for range of motion and look for areas up and down the spine that are tender or that are exhibiting nerve-related damage.
There will also be an assessment of sensations in other areas of the body to detect the presence of:
– tingling or a “pins and needles” feeling
– any numbness that may be present
– weaknesses and diminished reflexes
Other conditions like infections, tumors, fractures, strains, and muscle injuries will be ruled out, often by the use of imaging tests including X-rays and MRIs.
When a determination of degenerative disc disease is made, courses of treatment and intervention will be discussed. Strategies to cope with disc disease always begin with a conservative approach.
It’s important to remember that flare-ups of disc pain are highly episodic and heavily influenced by the presence of inflammation in the body. Early treatment will focus on coping strategies and pain relief with an eye toward behaviour modification and exercise to prevent future incidents.
Only in rarely and unusually severe cases is surgery recommended for degenerative disc disease, and then only after all other avenues have been fully explored.
Chapter 2: Disc Disease By Region
Degenerative disc disease differs according to the region of the spine involved. The areas most commonly affected, in order of occurrence are:
– lumbar or lower back
– cervical or neck
– thoracic or mid-back
Whenever possible, the symptoms caused by degenerative disc disease are addressed conservatively, with surgery an option of last resort only.
For the purposes of this discussion, we will look at the effects of disc disease starting with the neck and moving down the spinal column.
Cervical Disc Disease
Medical research indicates that approximately 67% of the world’s adult population will experience neck pain from cervical disc disease at some point in their lives.
Neck problems are especially common in later life due to accumulated damage to the vertebrae from decades of repetitive stress. Degenerative disc disease in the cervical region is more complicated than just experiencing pain, however.
Typically, as the discs in the neck begin to deteriorate, the person also suffers weakness and numbness in the shoulders, arms, and hands. This can lead to loss of flexibility and mobility that effects both work and leisure activities.
The Cervical Spine
The seven vertebrae of the cervical spine provide stability for the neck and allow for the smooth turning of the head. They support the least amount of weight, but are subject to greater stresses due to the extensive range of their mobility.
The vertebrae begin at the base of the skull and move downward to connect to the thoracic spine. They are designated as C1 through C7. The first vertebrae C1, forms a ring that rotates around C2.
Rotation, Flexion, Extension
The cervical vertebrae allow for rotation, flexion, and extension of the head and neck. Rotation is the movement of the head from side to side, which is primarily controlled by C1 and C2.
Flexion is the act of moving the head forward, while extension is the backward motion. This range is controlled by C5 through C7.
These basic motions, however, can occur in a huge range of sequences. Using our necks, we can look left and up, for instance, in a smooth curve.
Most of us give very little thought to just how smoothly these movements take place until they are interrupted. Then, when pain does surface, we are shocked at how much it affects our day-to-day lives.
Suddenly swiveling to check for oncoming traffic at a busy intersection is excruciating. However, if we don’t execute that motion, we risk being involved in an accident.
Under such real-life circumstances, the seriousness of neck problems becomes all too readily apparent. It is for this reason that people are often desperate to correct their neck pain, and wrongly assume that surgery is their only option.
Prevalence of Neck Problems
While it is more common to see disc degeneration in the lumbar spine, neck pain runs lower back pain a close second in prevalence.
Under the age of 40, only about 25% of the population develops signs of degenerative issues in the neck. From age 40 and beyond, however, the number jumps to 60%. This includes pinched nerves and the formation of bone spurs.
Types of Neck Pain
There are varying types of neck pain. Not all forms are associated with disc degeneration, but can rather be attributed to soft tissue injuries to the muscles, ligaments, and tendons.
Common causes of these complaints are auto accidents that result in “whiplash,” or getting a “crick” from sleeping the wrong way. Sometimes just carrying a heavy object will strain a neck muscle creating stiffness and soreness that can take as much as 2 weeks to resolve.
Pain that lasts from 2 weeks to a few months, however, is a sign that either a more serious injury has occurred, or that a degenerative disease is present. The common culprits are disc degeneration and arthritis, singularly or in combination.
Initial symptoms of neck problems of this type include loss of flexibility and stiffness or “tension” that is most often felt in the evenings.
Over time, the condition can continue to worsen until the discomfort migrates into the shoulders and arms. At this point, functional quality of life can be severely compromised.
Diagnosing Cervical Disc Disease
After taking a medical history and conducting a neurological exam, your doctor will measure your neck’s extension, and evaluate its flexibility.
Imaging procedures may be required, such as X-rays, an MRI, or a CT scan. These tests allow for a visual inspection of the condition of the vertebrae and spinal cord to help identify the origin of the pain.
These imaging scans will also reveal the presence of any arthritis, which may exist as a separate condition or in conjunction with disc degeneration.
Treating Cervical Disc Disease
The first line of defense in the early stages of cervical disc disease addresses reducing both inflammation and pain. In most cases, only over-the-counter medications are required.
The best options are non-steroidal anti-inflammatory painkillers including:
– acetaminophen
– ibuprofen
– naproxen
If these drugs don’t work, prescription steroids may be indicated. Some cases could require narcotic painkillers.
Regardless of the painkillers used, alternating applications of heat and ice can provide additional relief, and reduce how much medication has to be taken.
Physical therapy, including cervical traction and gentle manipulation are routinely used. Patients may work with a physical therapist, a chiropractor, a massage therapist, or some combination of all of these professionals.
Cervical collars and pillows are used to provide support during healing and are especially beneficial at night to improve the position of the head and neck. It is quite common for misalignment during sleep to exacerbate neck pain.
The overall goal of a complete therapy plan is to improve range of motion and posture while strengthening the supporting muscles of the neck. Cervical pain rarely remains constant throughout a person’s life, tending to be more episodic in nature.
Conservative treatment for a flare up of neck pain should lead to improvement of the condition within six weeks. Rarely is surgery required, but when it is, the predominant procedure is a discectomy.
Cervical Discectomy or Fusion
In severe cases of cervical disc degeneration, the diseased disc will be removed and replaced with an artificial metal disc (cervical discectomy) or by cervical fusion.
(Both procedures will be discussed in Part 3, which considers Standard Medical Treatments.)
When surgery is indicated, the standard period of recovery is three months to one year, followed by changes in lifestyle and habits to keep the intact vertebrae of the cervical region healthier.
Typically this includes exercise, eating a good diet, and stopping smoking if tobacco use has been a factor.
Thoracic Disc Disease
Thoracic disc disease is much less common than cervical or lumbar issues, but when it is present, it causes pain in the upper or mid-back regions.
There are 12 vertebrae in this section, which is that portion of the spine below the neck connected to the ribs. It is fairly common for a disc in this region to become herniated, exerting pressure on nerve roots or the spinal cord.
Disc disease in the thoracic spine does not always result in pain, however. In a controlled study with 90 pain-free patients, 73% showed clear evidence of disc degeneration and herniation.
This may suggest that when back pain is present in the thoracic region, the real cause is some sort of trauma to the upper back rather than the aging of the disc themselves.
Such injuries might occur as the result of a fall, or as a consequence of playing some type of sport.
If the pressure on the spinal cord is significant, spinal cord dysfunction or myelopathy can result. Symptoms might then include poor balance, weakness in the legs, and bowel or bladder dysfunction.
Thoracic Disc Herniation
Thoracic disc herniation presents with one of three potential patterns of protrusion:
– central
– lateral
– centro-lateral
Symptoms will differ in each case.
– With a central protrusion, pain is in the upper back, with a potential for spinal cord dysfunction depending on the size of the herniation.
– In instances of lateral protrusion, exiting nerves are most typically affected, with chest wall and/or abdominal pain resulting.
– Centro-lateral protrusions present with a combination of upper back pain, chest and abdominal pain, and potential spinal cord dysfunctions.
Symptoms are always further delineated by the size and location of the disc.
Diagnosing Thoracic Disc Disease
Patients with problems in the thoracic spine report isolated and/or radiating pain in the upper back that may be worse when they cough or sneeze.
Since pain in this region may also be indicative of heart and lung problems, as well as kidney and gastrointestinal issues, it’s imperative to get a clear diagnosis of the source of the discomfort.
After taking a full medical history, the doctor will conduct a physical examination and attempt to evaluate both the location and severity of the pain.
The best avenue for accurate diagnosis, however, is the use of imaging tests like X-rays or an MRI. The latter is especially good to find bone spurs or to locate a herniated disc.
X-rays may be taken as part of a myelogram, which involves injecting dye into the spinal column to precisely identify areas of pressure.
If an MRI is not an option for any reason, a CT scan will likely be ordered.
Treating Thoracic Disc Disease
Under the direction of a physical therapist, a program of low-impact aerobic exercise and core strengthening is the first line of treatment for thoracic disc disease. Both walking and bicycling are standard options.
An initial period of complete rest may be ordered, with subsequent modification of activities that seem to worsen the condition.
Over-the-counter non-steroidal anti-inflammatory pain medications are preferred to narcotic drugs, and alternating applications of heat and cold may be helpful. Many patients report significant pain relief and improvement via chiropractic manipulation.
In some instances, epidural injections of steroids are ordered to lower inflammation in the region. All of these approaches should be paired with back-strengthening exercises.
Surgery is typically indicated only when significant bone spurs are present that are compressing the spinal cord and causing neurological symptoms like tingling, numbness, and weakness in the legs.
The goal of the surgery is to remove the compression and may involve the use of rods or plates to limit or stop motion in the problem region. If the diseased disc is removed, a bone graft or other device may be put in its place to facilitate bone fusion and healing.
There are no total disc replacement prosthetics for the thoracic spine like those used in the cervical spine or neck.
(Thoracic procedures will be discussed in Part 3, which considers Standard Medical Treatments for degenerative disc conditions.)
Lumbar Disc Disease
Although the lumbar region is comprised of only five vertebrae, it is the most likely area of the spine for disc degeneration to be present.
Lumbar disc disease with attendant lower back pain is the second most common reason patients see their primary care physicians, and the fifth most common reason for scheduled appointments with orthopedists.
In the developed world, estimates suggest that 60% to 80% of all adults will experience lumbar disc disease as they age, a condition easily exacerbated by injury and obesity.
Diagnosing Lumbar Disc Disease
Lumbar disc disease carries a range of clear symptoms. It presents with continuous low-grade pain that necessitates only mild palliative measures.
From time to time, however, there will be intense flare ups that are much more problematic, and may increase in frequency as the individual ages.
Symptoms of lower back disc degeneration include:
– Aching pain in the center of the lower back with radiating sensation into the hips and legs.
– Pain that is present for more than six weeks.
– Lower back pain that is more intense when sitting as opposed to standing, walking, or lying down.
– Pain aggravated by prolonged standing, bending forward, or picking up an object.
– More intense pain when twisting, lifting, or bending.
– Numbness and/or tingling in the legs, which can include difficulty walking.
In some cases of collapsed disc, the exiting nerve root may become pinched causing severe, shooting pains in the affected leg.
Your doctor should take an extensive medical history and ask that you describe not just your pain and symptoms, but also your daily activities.
This will include questions about physical positions, overall posture, repetitive movements, amounts lifted, and duration of times standing and sitting.
In a physical exam, your range of motion and muscle strength should also be evaluated along with any localized tenderness. Typically an MRI will be ordered both to pinpoint the location of the diseased disc and to rule out any other potential causes of the discomfort.
Treating Lumbar Disc Disease
For the most part, lumbar disc disease can be treated conservatively without surgery using over-the-counter medications to control pain and inflammation.
Alternating hot and cold packs are a standard strategy for greater comfort. In more severe cases, epidural injections of steroids are also effective.
Surgery is typically only considered if no relief has been achieved after six months, or if the pain is significantly affecting the patient’s life.
It’s important to identify aggravating activities and to modify or eliminate them from the daily or work routine. Many patients benefit from learning the correct way to lift, as well as how to design more ergonomic working and sleeping spaces.
A program of exercise designed by a physical therapist can facilitate pain relief, improve posture, and strengthen the surrounding muscle structures. Some patients also find working with a chiropractor to be tremendously helpful.
Want to read the entire thing?